“The fact that you were able to perform [1,642] operations with the tremendous results that you have had should be not only gratifying to you but gratefully received by our profession.” —Cecil O. Samuelson, M.D. (Dean, School of Medicine, University of Utah; In a letter to Calvin Midgley, 4 Dec 1987)
In 2004, 11,892 women in the U.S. were diagnosed with cervical cancer, and 3,850 women died from the disease (US Cancer). Worldwide, it is the second most common cancer contracted by women older than 15 (as qtd. by Soong). The methods currently used to treat precancerous cervical growth without causing infertility are only marginally effective (Bickford et al.), and the need for a better method of detecting cervical cancer has been officially recognized (Bickford et al.). Another extremely common set of ailments women experience are significant, long-lasting discomforts and complications from delivery of children. In the mid 1800s, T. A. Emmet, an obstetrician, reported, “Fully one-half of the ailments a woman complains of, who has borne at least one child, are due to a laceration of the cervix,” (as qtd. by Midgley, Problems.). Surprisingly, the simplest imaginable solution for these problems has been under the noses of medical professionals for over 70 years and easily outperforms the current treatments for cervical damage (namely cauterization and conization).
In 1930, young and talented medical practitioner Calvin Midgley married the girl of his dreams—despite learning that she would probably die if she tried to have children because she had a weak heart. He promised he would take care of her, and that if she wanted children, she would have them. Elsie lived through delivery, but severe post-natal complications due to the rough delivery of a first born in 1932 caused Elsie substantial ongoing discomfort. Joanne was a breech baby, feet first, causing a prolonged, extremely difficult forceps delivery (Midgley, E. interview 1). Midgley observed these traumatic deliveries taking place on other women as well and was inspired to research ways to repair the damage done by violent birth.
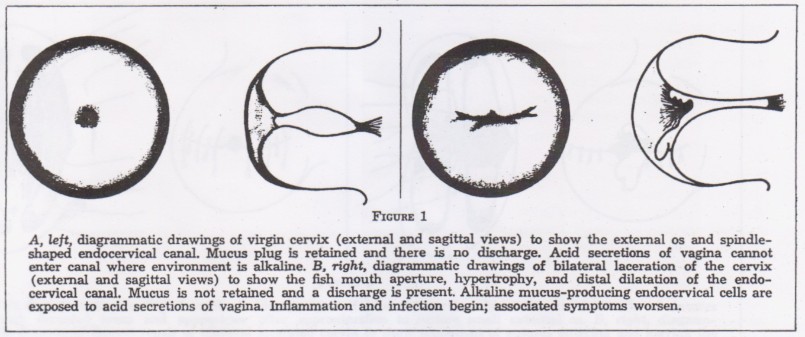
The interior of the virgin cervix is a cylindrical tube, with a bulb-like space immediately before the opening of the cervix (Diagram 1, from Midgley et al. Semilunar). In a healthy cervix, this space contains a mucus plug. The mucus plug hydrates the cervical tissue and prevents infections from invading foreign particles, bacteria, and the acidic environment of the vagina. The shape of the cervix allows the mucus secreted by the cervix tissue to be retained. After a woman bears a child, the neck of the cervix is stretched and/or torn, and the shape of the cervix becomes long and uninterrupted (Midgley, Video). The secreted mucus leaks from the cervix and is no longer able to prevent infections. The cervix often becomes irritated and inflamed. Constant or frequent discharge, backaches, menstrual irregularity and infertility are common symptoms of cervical damage (Midgley et al. Semilunar).
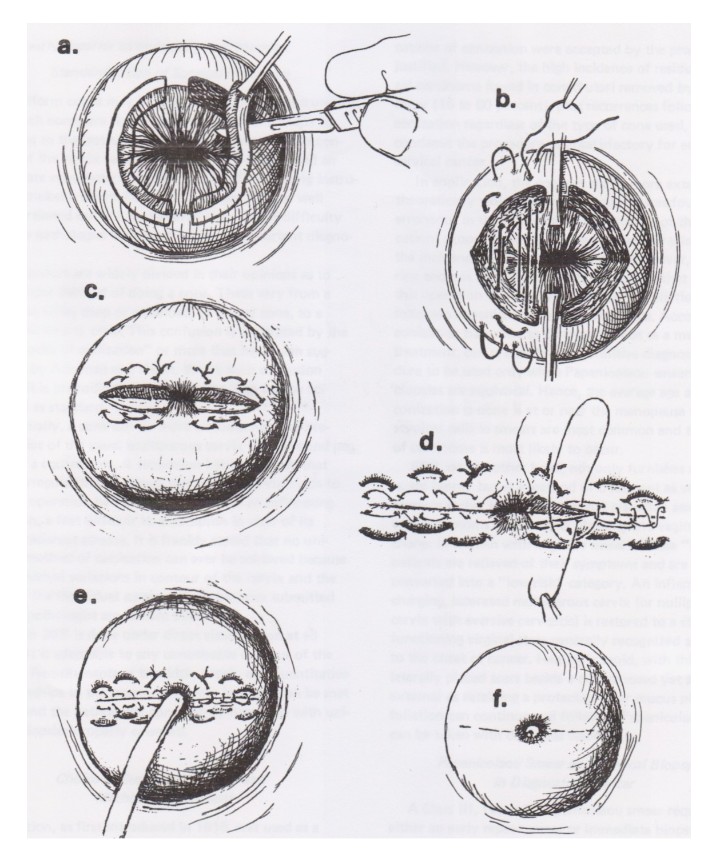
The purpose of the procedure invented by Midgley—Semilunar Biopsy Repair (SBR)—is to return the cervix to a virgin state. This innovative operation is extremely simple and can be performed in 30 minutes, with a local anesthetic, in an office setting, on an out-patient basis (Midgley, Video). Triple sulfa antibiotic ointment cream is applied to the absorbable stitches at the end of the procedure to prevent infection (Midgley et al. Alternative). The cervix usually heals completely within 2 weeks, before the next menstrual period (Midgley et al. Alternative). The inflamed tissue that was cut from the cervix is sent to a lab to be tested for abnormal or pre-cancerous cells (Midgley, Video). In the first publication by Midgley on SBR in 1971, he reported that of 843 patients, only 58 (6.8%) experienced post-operative hemorrhage requiring additional surgery (Midgley et al. Semilunar). The surgery is gentle enough that it can be performed multiple times without damaging the opening of the cervix (a.k.a. the OS) if the procedure is needed again (Midgley et al. Surgical).
Semilunar Biopsy Repair was invented in 1938, and Midgley
performed it over 1,642 times during his career. Short-term benefits include
significant reduction in vaginal discharge (131/161 completely relieved, 19
improved) and backaches (78/116 completely relieved, 13 improved). Even if all
the symptoms were not alleviated, the surgery was still considered to be
valuable to the patients because it increased the cervix’s ability to prevent
and fight infection. Out of all his patients, only two women were reported to
have developed cervical cancer, even though multiple women (6/843 in 1971
report) were diagnosed with partially developed cervical carcinoma (malignant cancer)
at the time of surgery
(Midgley et al. Semilunar). A statistical analysis was made to determine the
percentage of patients that should normally have developed cervical cancer, and
it appeared to demonstrate that receipt of SBR converts patients from a
high-risk category to a low-risk category. It is also significant that the two
woman who developed cancer waited 2 and 7 years respectively after cervical
laceration to receive SBR; Dr. Midgley felt that had they received the surgery
sooner, onset of carcinoma might have been prevented (Midgley et al.
Incidence). Eroded non-parous cervixes (cervixes that have never given birth to
a child) also benefit from this procedure, and there is reliable evidence that
SBR improves fertility whether or not a woman has already borne a child
(Midgley et al. Incidence).
Although Dr. Midgley was an extremely reputable doctor (in his entire career of 57 years, he never had a single malpractice suit filed against him), his technique did not attract much attention because he was a general practitioner. At the time, the medical community was only willing to entertain the innovative ideas of specialists. Since Midgley was neither an obstetrician nor a gynecologist, his invention was stigmatized and largely ignored. After his retirement, Dr. Midgley donated a substantial sum to the University of Utah to study the technique further, but grew impatient at the university’s pace and asked them to return the grant so that he could pursue research elsewhere. (Details of the closing report were not available.) Although Midgley was unable to privately conduct sufficient research to attract ongoing interest in his project, other doctors who had assisted or watched Midgley operate recognized the potential of the surgery and began performing it in secret, attempting to take credit for its invention. Midgley later learned about these extra operations from the thrilled patients (Midgley, E. interview 2). Despite the enormous success of SBR on the table, it was never accepted by the medical community at large, nor approved by the United States government. Dr. Midgley died in 1994 (Obituary), somewhat frustrated.
Historically, the woman’s cervix has been subjected to significant disservice. In the 1800s, to assist in the ease of birth, doctors used to lacerate the cervix with a knife to widen the opening (Midgley, Video). Partial or complete amputation of the cervical opening has even been employed in attempts to alleviate discomfort associated with cervical lacerations (Midgley et al. Semilunar). In 1862, Emmet recognized the problem and invented a cervical repair procedure. Unfortunately the surgery was poorly tested before being widely performed. It was discovered too late that the Emmet repair had high risks and low benefits. Complications and/or infections were common, and the likelihood that pre-surgery symptoms would improve was low (Midgley et al. Semilunar).
The most common treatment used today is cauterization of the cervix, invented by Hippocrates some 2,500 years ago. Some medical professionals have called cauterization of the cervix “distressing” since the early 1900s (Moss, Cauterization), but this method is still used today as the best known treatment for certain kinds of cervical damage, for pre-cancerous lesions of the cervix, and for erosion of the cervix, known as cervical erythroplaquia. One cauterization procedure consists of applying a red-hot rod to the OS and cervical canal to completely char all diseased cells 3-4 millimeters deep in every direction (Kelly). The result is a “black, unsightly cervical mucosa” (Kelly), no longer capable of secreting mucus to hydrate and protect the cervix (Midgley, et al. Surgical). A cervix may also be cauterized with electricity, liquid nitrogen, or other chemicals, with the objective being to thoroughly burn the cells of the cervix. Cautery is administered multiple times before treatment is considered complete (Kelly). Cautery may also cause scarring, hindering pap smear diagnosis in the future. Scarring can also result in a hardened cervix that would make childbirth more difficult, because the cervical canal cannot dilate properly. There are indications that cauterization itself may increase the likelihood of contracting cervical cancer (Midgley et al. Surgical).
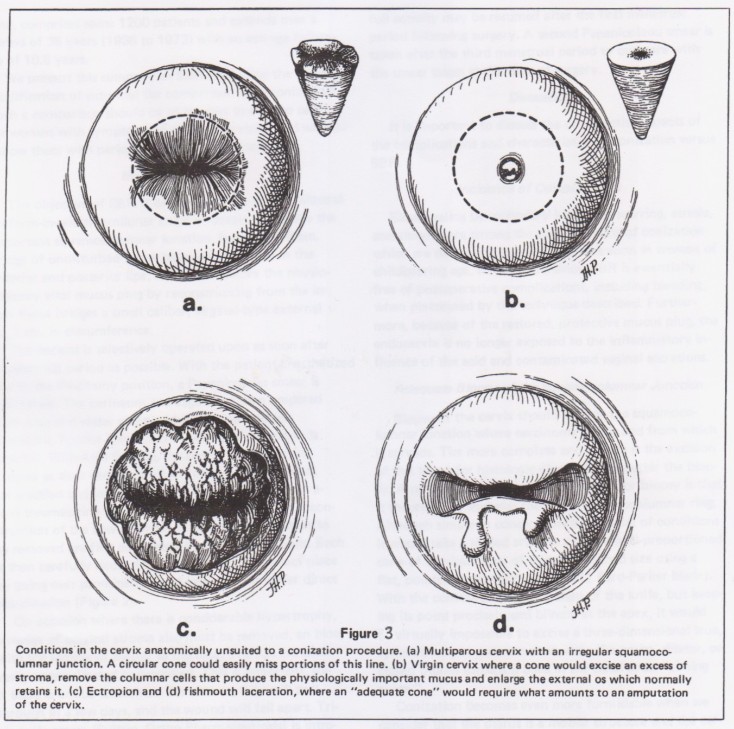
Conization is another extremely common procedure, but its risks are so high that it is only performed after multiple tests indicate cancerous or pre-cancerous cell growth in the cervix (Midgley et al. Alternative). In the procedure, a cone-shaped chunk is cut from the OS (Diagram 3, from Midgley et al. Alternative), leaving the interior cervix completely exposed to the acidic environment of the vagina. This procedure was originally condemned because of serious complications associated with it. It was re-approved with the acceptance of pap-smear tests in 1943, because a method of biopsy was necessary. The cone cut from the OS provides pathologists with a biopsy that sheds further light on the actual condition of the cervix in relation to the state of carcinoma. It was hoped that conization would also provide a treatment for cervical cancer. However, the likelihood that incomplete excision (partial removal of the cervix as opposed to complete removal of the womb) will actually improve the cancerous condition of the cervix is questionable at best (Ghaem-Maghami et al). Conization also requires an extremely long recovery period of 6-10 weeks. SBR could completely replace conization; it fills every need. SBR can be performed in many cases where conization cannot (Diagram 3, from Midgley et al. Alternative). It provides an equivalent biopsy without inflicting the irreparable damage caused by conization. SBR is significantly simpler, less intrusive, heals faster, and has undisputedly superior success rates without the substantial risks of conization.
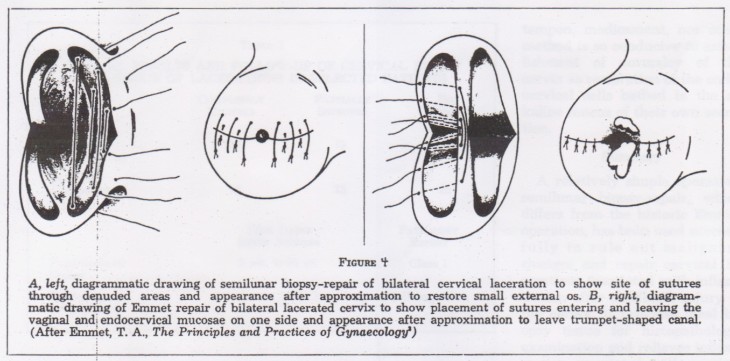
Part of the medical community’s resistance toward SBR is because the procedure is similar in appearance and method to the unsuccessful Emmet procedure from 1862. In both surgeries, the inflamed epidermis on the lip of the OS is cut away, and the exposed tissue is sutured together (Diagram 4, from Midgley et al. Semilunar). However, in the Emmet procedure, the cervix is deliberately reconstructed to provide a trumpet-shaped OS with a large opening, theoretically to improve the ease of future births. In contrast, the SBR procedure restores the opening to a diameter the same size as a clinically virgin cervix (Midgley et al. Semilunar). The shape of the cervix restores the bulb of mucus, whereas the Emmet procedure does not retain the mucus plug, leaving the cervix vulnerable to further infection. The virgin size of the OS does not impair sexual intercourse, and actually improves fertility. The comparatively small OS also never resulted in difficult or abnormal childbirth or labor in post-SBR pregnancies, which typically occurs in one in five human labors.
There is currently no evidence refuting the claims made by Dr. Midgley. While lack of negative evidence does not by any means imply that SBR is perfect or that it should be immediately practiced without further scrutiny, the four publications in favor of SBR and 1,642+ operations with overwhelmingly positive results demand the attention of the medical community. SBR should be lifted out of obscurity and no longer ignored as it has been since Midgley’s death.
The implications of Semilunar Biopsy Repair are monumental. Generations of women have needlessly endured physical and emotional trauma—and death—due to a simple problem with a simple solution. The restoration of the cervix to the natural order of its creation, the condition where it is naturally equipped to protect itself and fight infection, should have been the objective since the health problems associated with cervical lacerations were discovered. It should be obvious that pink, healthy tissue is infinitely preferable to a charred, scarred cervix that is no longer inflamed only because the cells are dead. The evidence supports the procedure. Therefore, the procedure should be further studied and, as Samuelson said, gratefully accepted by the medical community.
Women who currently experience the symptoms described should educate themselves about the risks and benefits of SBR. If they then desire the procedure, they should request it from a competent medical professional. History demonstrates that significant medical advancements are often mocked by the world at large when first introduced. Cancer-diagnosing pap smears, the polio vaccine, and antibiotics for ulcers are prominent examples of this tendency. Often, it is not until educated individuals demand the innovative treatments for themselves or their family members that the life-changing, life-saving advances have been accepted by the world at large (Midgley, Letter).
Works Cited
Bickford, L.R.; Drezek, R.A.; Yu T.K.. “Intraoperative techniques and tumor margin status—room for improvement for cervical cancer patients of childbearing age”. Gynecology Oncology. Vol 107. P. S180-186. Published October 2007.
Kelly, Howard Atwood. “Medical Genecology”. New York and London, Publisher: D. Appleton and Company, 1908. P. 270.
Ghaem-Maghami, S.; Sagi, S.; Majeed, G.; Soutter, W. P.. “Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis”. The Lancet Oncology. Vol 8, Issue 11. P. 985-93. Published November 2007.
Midgley, Calvin P.; Sommer, Robert W.; Armstrong, Gerald. “An Alternative to Conization: Semilunar Biopsy Repair”. Clinical Medicine. Vol. 78. P. 15-18. Published September 1971.
Midgley, Calvin P.; Sommer, Robert W.. “Semilunar Biopsy and Repair of the Uterine Cervix After Childbirth”. Clinical Medicine. Vol 82. P. 13-18. Published January 1975.
Midgley, Calvin P.; Armstrong, Gerald. “Surgical Prevention of Cancer of the Uterine Cervix”. Clinical Medicine. Vol 84. P. 16-22. Published December 1977.
Midgley, Calvin. Letter. “Problems with medical care”. The News Sun. 28 Feb 1980.
Midgley, Calvin P.. Video footage of Semilunar Biopsy Repair procedure. Viewed 21 March, 2009.
Midgley, Wendy; daughter of Calvin Midgley. Email interview. 5 April 2009.
Midgley, Wendy; daughter of Calvin Midgley. Email interview. 16 April 2009.
Mind Your Body Feb Issue 2008, as qtd. by Alvin Soong. “Things you should know about cervical cancer”. Published online 29 Feb 2008. Retrieved 9 April 2009.
Moss, Lawton E. “Cauterization of the Cervix” British Medical Journal. 1(4023): 361. Published 12 February 1938.
Obituary of Calvin Midgley. Copy of original, publication information unknown.
U.S. Cancer Statistics Working Group. United States Cancer Statistics: 2004 Incidence and Mortality. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; Published 2007.
This summary has been adapted from a research paper written by Laura Shanae Crenshaw for a writing class at Brigham Young University. In 2010, BYU awarded the paper first place for research papers in an Honors writing contest. Information on Midgley's Semilunar Biopsy Repair procedure was previously unavailable to the public.